While not a new concept, force transmission remains a relatively unknown commodity amongst manual therapists. My good friend and colleague Dr. Michael Chivers lectures on the subject frequently, as do several others. Yet it remains a fairly obscure topic in most circles.
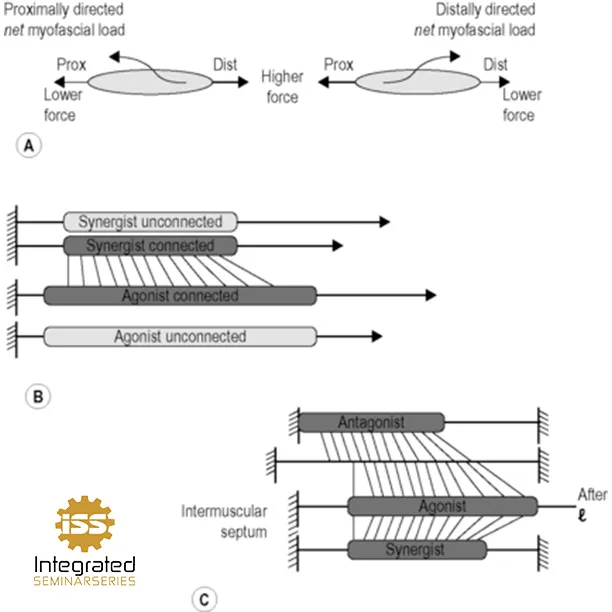
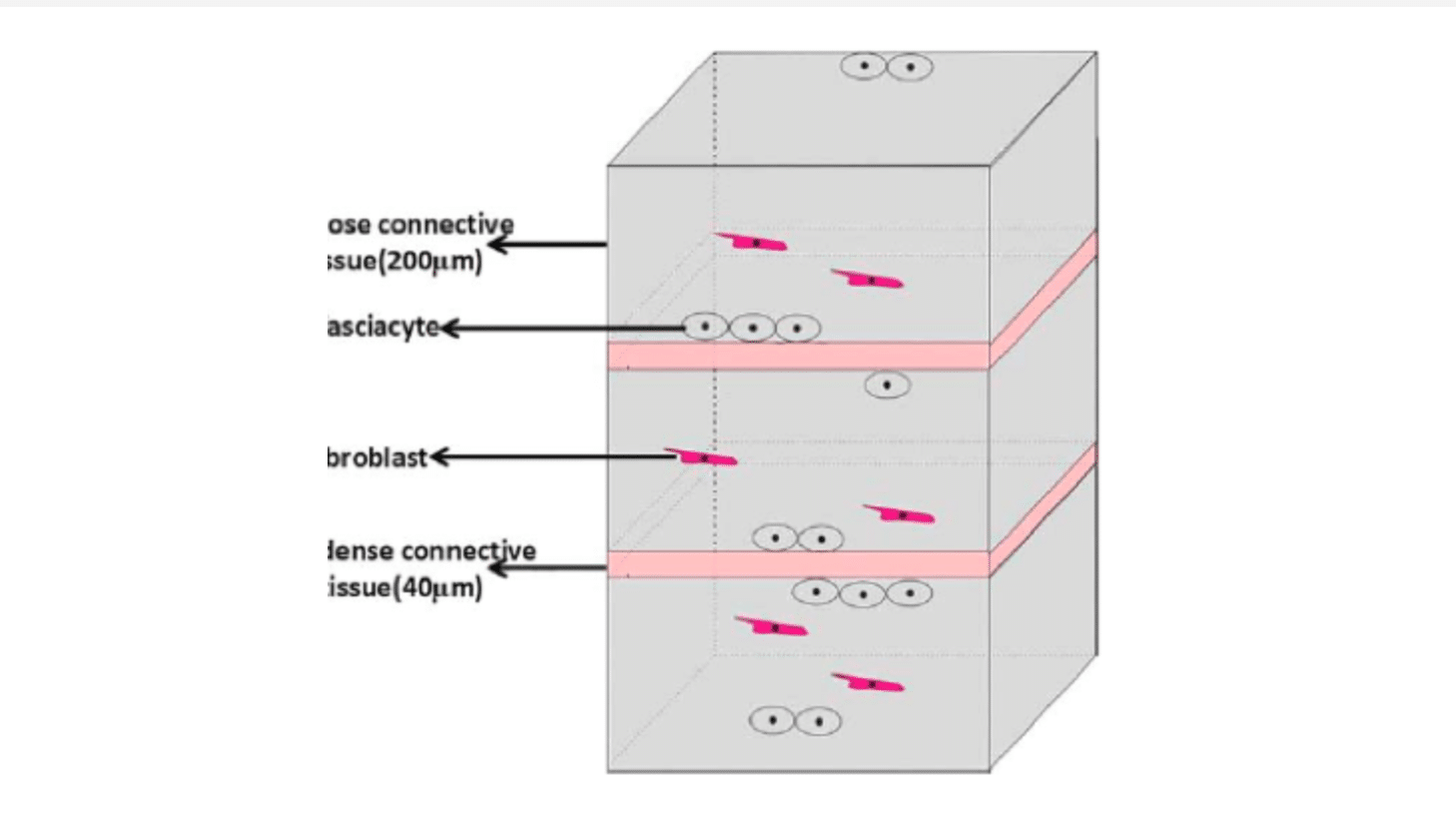
Several papers over the past 15 years have documented that, in addition to myotendinous force transmission, conduction of forces also occurs via alternative pathways, between muscles and between muscle and non-muscular tissues. Force is transmitted onto the connective tissue stroma of the muscle where there are several paths available for further transmission, meaning that all force will be exerted at the muscle own tendons. The relative stiffness of each pathway will determine the fraction of force transmitted through them – increased stiffness means increased transmission. Through the epimysium, force may be transmitted directly between synergistic muscles, but may also occur via indirect pathways involving the neurovascular tract. This latter route is perfect given that the relative stiffness of neurovascular tracts makes them particularly suited for such transmission. In addition to intermuscular effects, force transmission between muscle and non-muscular structures are expected. Neurovascular tracts once again play an important role in this mechanism, as they are not only connected to muscle, but also via the periosteum to bones, either directly or by way of other fascial structures to which it may be connected, including interosseal membranes, intermuscular septae or even the general fascia.
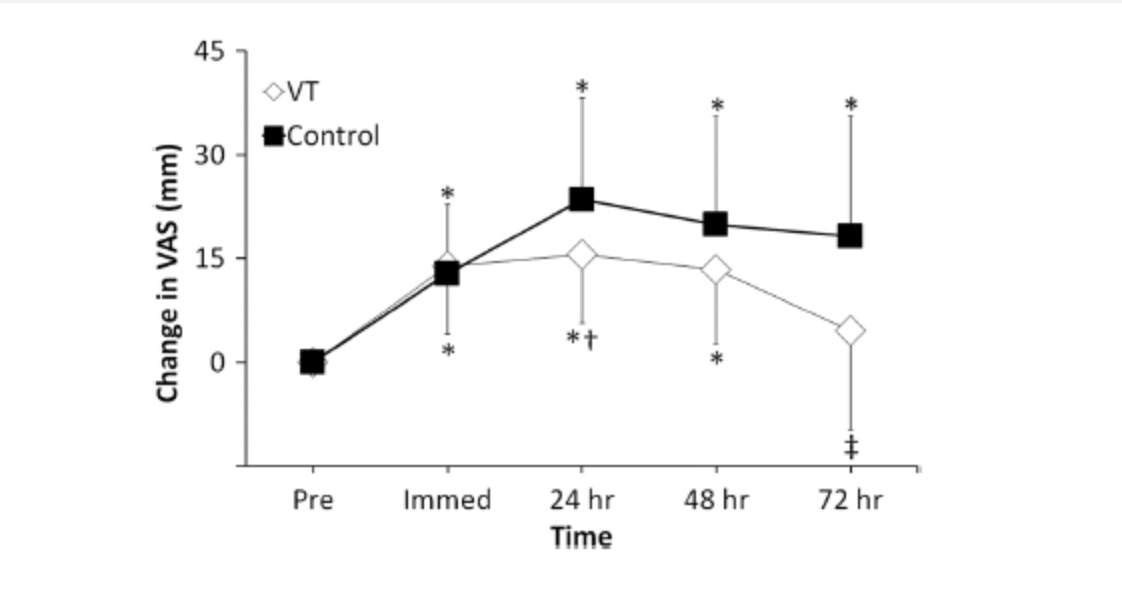
One of the earlier papers by two of my favorite authors on the subject, Huijing and Yucesoy, in Surgical and Radiological Anatomy 2011, is the first dealing with human subjects (their earlier work involved rats). The authors used MRI to measure strain that occurred in the soleus muscle with knee flexion, while the ankle remained in a rigid foot ankle orthosis brace. Specifically, for determination of globally induced strain in the gastrocnemius, knee joint angles were imposed, while keeping ankle joint angle constant and measuring its muscle–tendon complex length changes. In vivo local strains in both the gastrocnemius and soleus were calculated using MRI techniques in healthy human volunteers comparing images taken at static knee angles of 173 and 150 degrees.
Below is a pictorial representation of the set up Huijing and Yucesoy used can be seen here:

If the soleus and gastrocnemius muscles are fully independent mechanically, no local strains should be encountered within soleus muscle since it does not cross the knee joint and as such no global strains are imposed on this muscle–tendon complex. However, the authors noted considerable strain within the soleus muscles, both lengthening and shortening in response to the knee extending and flexing, respectively. They therefore concluded that there were considerable mechanical interaction between these synergistic plantar flexor muscles. These local changes in strain are inexplicable unless intimate connections between these synergistic muscles are assumed that transmit force between the gastrocnemius and soleus.
What is the take home message? The major results of this study are the findings that local strains within the muscle are very much higher that the global strains imposed on it, and such local strains are not limited to the specific muscle that is exposed to length changes, but also occur within synergistic muscle kept at constant muscle–tendon complex length (global isometric condition). This means that synergistic muscles are not mechanically independent.
The essence of the concept of myofascial force transmission is that force transmission of muscle is not limited to that between a specific muscle and its own tendons; rather a portion of the force generated is simultaneously transmitted ‘‘sideways’’ between muscles, either directly between adjacent muscle bellies (intermuscular transmission) via the shared epimysium between said muscles, or via extramuscular connective tissues linking synergistic muscles and between muscle and bone (extramuscular force transmission). The specifics of force transmission from an anatomical perspective, can be summarized as follows: the sarcomeres within muscle fibers are connected to the intracellular cytoskeleton that is connected via subsarcolemmal actin filaments to trans-sarcolemmal molecules (most notably integrins and/or sarcoglycans) that is connected to the endomysium, a connective tissue tube within each muscle fiber is located. The collection of endomysial tubes of a muscle fascicle form a continuous system that is surrounded by another connective tissue tube – the perimysium. Groups of small fascicles or bundles of muscle fibers are surrounded as well by epimysial tubes. In turn, the collection of perimysia constitutes a continuous system, sometimes called a stroma that is delimited by the epimysium. In vivo muscle is working within its natural context of connective tissues. For synergistic muscles, walls of epimysial tubes are shared, except for places where neurovascular tracts passes between muscles. However, neurovascular tracts also connect muscles to each other as branches containing vessels and nerves pass into the muscle and are continuous with the tertiary perimysium that does not fully surrounds fascicles or groups of small fascicles. The neurovascular tracts are attached also to the periosteum surrounding the bones and to other non-muscular elements of the connective tissues system, such as the interosseal membrane, the intermuscular septum which themselves are continuous with the general fascia of the limb. This describes the full continuity of the system. However, if myofascial force transmission will occur to an appreciable extent using a specific pathway, is not so much determined by the fact that it is connected, but rather the actual stiffness of the connections, which depends on the actual circumstances such muscle length (i.e. joint angle) and relative positions of muscles with respect to each other and to the non-muscular elements described above.
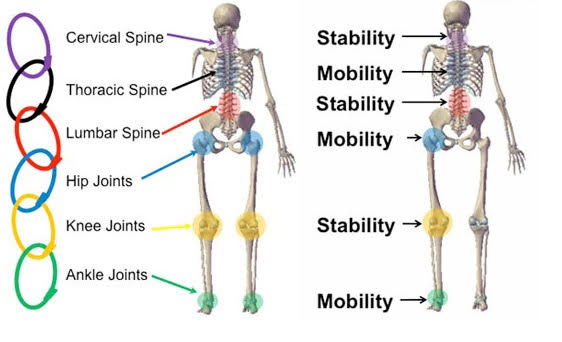
As a doctor or therapist, what are the clinical implications of force transmission? The current research shows that tension can be transferred between at least some of the examined adjacent muscles, which challenges the traditional view that muscles function as independent actuators during physiological movements. This view point has also been supported by Herbert et al 2008, Maas & Sandercock 2008 and van der Wal 2009. The possibility of load transfer between muscles encourages targeting entire myofascial chains in the evaluation process, therapy and exercise. Instead of focusing on single structures, muscles or joints, more holistic diagnostic and treatment approaches seem appropriate for overuse conditions or radiation pain symptoms that involve several structures of myofascial chain. In a series of experiments in rats, Rijkelijkhuizen et al 2009 have shown that such mechanisms and effects are active between all muscles of the lower leg. So even antagonistic muscles located at opposite sides of the leg interact and cannot be considered as fully independent entities. It should be realized that this means that part of the force exerted by active sarcomeres within a muscle may be exerted at the tendon of its antagonistic muscle.
Assess globally. Treat globally – from both a mechanotherapy and exercise perspective.