Understanding the Connection Between Lower Extremity Function and Low Back Pain: A Biomechanical Approach for Effective Treatment
When I ask attendees at the beginning and at the end of our Integrated Assessment and Integrated Patterning seminars “how would you treat this patient with facet synovitis low back pain?” I get incredibly different answers. While therapists have a solid foundation in terms of managing symptoms, we unfortunately do not have a concomitant understanding of pathomechanics. Low back pain, in the absence of a single traumatic episode, is orders of magnitude more common in our offices than patients who have been subject to a single traumatic episode. Think of this in terms of your car not starting. If you get into an accident and your car does not start, the answer is simple – you sustained a single episode of vehicular trauma. The parts need to be repaired. But what if you try and start your car in the morning and find it will not drive? No “trauma” has occurred. A patient with low back pain is the human equivalent of a car that will not start. Many people have low back pain, but do they all have no back pain for the same reason? Logic dictates that this is not plausible, in the same manner that every person who has a car that will not start experiences it for the same reason. Follow this analogy to the “treatment” aspect of both scenarios. Are you comfortable leaving your car with a mechanic who tells you they will do small amounts of 5-6 things that have shown to be effective in managing a car that will not start? Unequivocally the answer is no. You want the technician to find the reason for your car not starting and fix that single aberration. Why then do we not employ the same rationale in dealing with low back pain? Instead of providing a smattering of interventions which have been shown to have some utility in managing back pain, would it not be more prudent to assess all the factors that may contribute to that pain and provide therapy on only those which are influencing the diagnosis? This seems like a far more pragmatic approach to the problem, and one that is germane to other professions but is absent in the realm of therapy.
Unveiling the Causality Conundrum: The Overlooked Factor in Therapy
The other issue with therapy as it pertains to all conditions is that we are not taught to appreciate causality. Moving away from the car metaphor, consider two employees who work at a distribution centre. Their boss tells them they need a total of 20 hours of work from them each day. Employee 1 does not want to work there, and contributes 3 hours of work each day, while employee 2 is left to contribute the remaining 18 hours. At the end of the month, employee 2 is sore, tired, injured, and generally run down. Employee 2 exhibits symptoms, like a lumbar spine will exhibit symptoms, when it has been overloaded. Which of these two employees is the “problem?” Clearly employee 1, who is causing employee 2 to become overloaded. Taking this back to low back pain, do we routinely assess our patients to determine why their lumbar spine is being overloaded? If we are not, we are missing causality. Is it safe to assume that every person with low back pain has the same areas contributing to lumbar spine overload? That is like assuming every case of a car that will not start is caused by the same issue, which we know to be false. Consdier as well the research of Abenhaim et al. who noted that only a small percentage of individuals with LBP have an identifiable pathoanatomical source, and the multiple studies indicating the potential inability of diagnostic imaging to identify the pain source, influence prognosis, or affect outcomes.
Is there proof that this sort of relationship exists? We will consider the relationship between the hips and the lumbar spine and investigate the literature therein.
The Role of Regional Interdependence in Manual Medicine
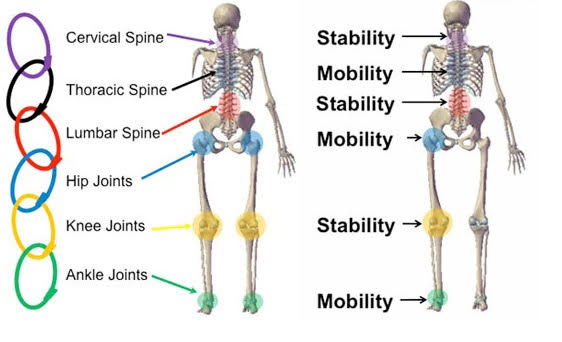
While research has demonstrated the effectiveness of subgrouping patients into a classification system based on signs and symptoms indicating their likelihood to respond to specific treatments. This classification approach has produced improved outcomes and high levels of reliability as compared with clinical practice guidelines; however, many patients will fit into a treatment-based subgroup. Prediction rules, as outlined here, are meant to classify patients to specific treatments; their purpose is not to explain how or why the variables influence the outcome. Therapists must then rely on an impairment-based approach, identifying potential local or remote contributors to the patient’s area of primary concern. Recent advances in research have begun to indicate the importance of this regional approach to musculoskeletal examination, but the contributing areas remote to the lumbar spine have yet to be fully elucidated. Given the biomechanical relationship between the hip and the low back, specifically the multiple shared muscles, one must consider the hip joint a potential contributor to low back pain. Contraction of these muscles will affect motion at the spine, pelvis, and hip because of common attachment sites. It is generally understood that movement at one of these areas will necessitate compensatory movement at the others because of these common muscle attachments and the concept of regional interdependence as indicated by Wainner et al. in 2007.
“With respect to. musculoskeletal problems, regional interdependence refers to the concept. that seemingly unrelated impairments in a remote anatomical region may. Contribute to, or be associated with, the patient’s primary complaint”
- Wainner et al, 2007
Regional interdependence as it applies to musculoskeletal physical therapy refers to “the concept that seemingly unrelated impairments in a remote anatomical region may contribute to, or be associated with, the patient’s primary complaint.” By understanding the association between the hip and low back, clinicians might gain insight into the management of this challenging patient population.
Understanding the Biomechanical Link between Hip Joint and Lumbar Spine: Implications for Hip-Spine Syndrome and Low Back Pain
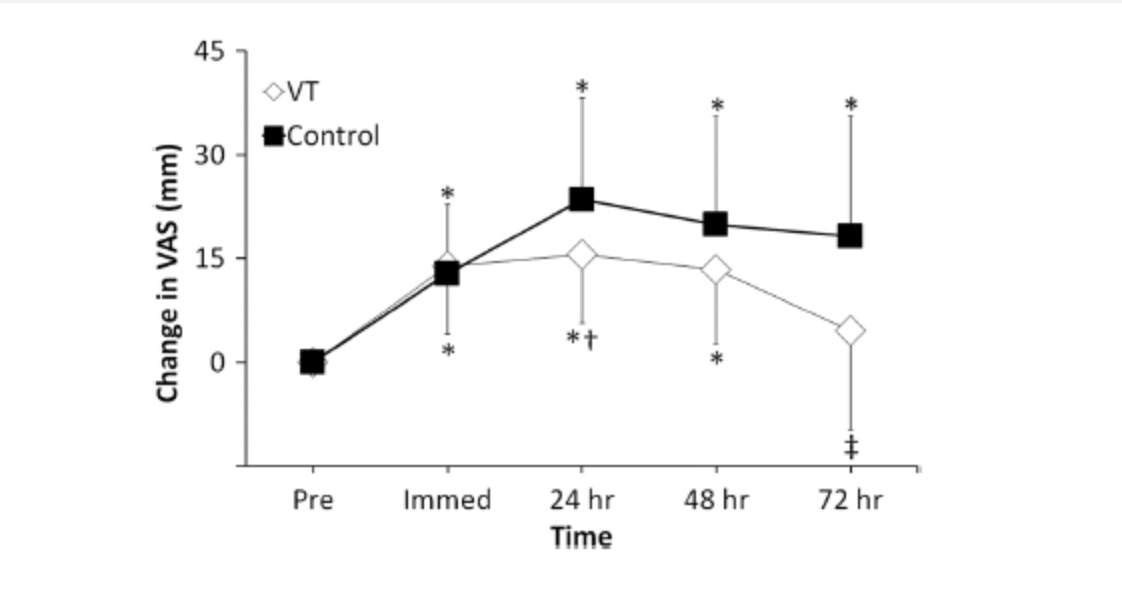
This concept of a biomechanical/pathomechanical link between the hip joint and the lumbar spine has been described as hip–spine syndrome (HSS). HSS specifically depicts the influence of a pathological hip joint on the alignment of the spine and subsequent muscle length and joint forces as noted by Offierski and McNab in 1983. More recent documentation of this relationship has been that of severe hip osteoarthritis (OA) causing abnormal spinal sagittal alignment and ensuing LBP. Ben-Galim et al. evaluated the effects of surgical treatment of hip OA on low back disability in patients preoperative and postoperative total hip replacement and found significant improvements in both visual analog scores for LBP and Oswestry Disability Index scores after surgery that remained at the 2-year follow-up.
This proposed regional relationship has been further substantiated through numerous studies. Ellison et al. compared the hip rotation of patients with LBP with that of unmatched controls without LBP. Patients with LBP more frequently demonstrated asymmetrical hip-rotation ROM, with internal rotation (IR) being less than external rotation (ER). Chesworth et al. also compared hip-rotation ROM in subjects with LBP with a control group matched for age, gender, height, and weight. Both IR and ER were significantly limited in the LBP group compared with the control group. Cibulka et al. observed subjects with LBP to have bilateral asymmetries in hip IR, whereas patients with LBP and sacroiliac-joint dysfunction had unilateral asymmetries. A cross-sectional study by Vad et al. demonstrated that symptomatic, as compared with asymptomatic, professional golfers had significantly decreased hip ROM in a combination of flexion, abduction, and external rotation (FABER) of the lower extremity that leads in the golf swing when compared with the opposite leg. In addition, these same symptomatic golfers had significantly decreased hip IR ROM of the lead leg compared with the non-lead leg (11.8° vs 16.9°, respectively). No hip ROM asymmetries were reported in the asymptomatic subjects. The aforementioned studies support the idea that restricted ROM, whether pathological in the case of hip OA or nonpathological in the case of soft-tissue restrictions, are correlated with LBP.
The Link Between Hip Muscle Strength and Low Back Pain: Insights from Athlete Studies and Beyond
We enter into a more interesting discussion when we look at the researching concerning muscle strength in the hip and its relationship to low back pain. The work investigating the effects of hip strength on LBP has focused primarily on athletes. In 2000, Nadler et al. examined the relationship of hip-extension and hip-abduction strength in athletes and their effect on future LBP and lower extremity injury. Female athletes with a history of LBP demonstrated a significant side-to-side asymmetry in hip-extensor strength, while no difference was found in hip-extensor strength for male athletes with or without a history of injury or in hip-abduction strength differences for either gender. In 2001 Nadler et al, examined hip-abductor and hip-extensor strength in college athletes. Logistic-regression analysis indicated a difference in side-to-side hip-extension strength as a potential predictive variable of future treatment for LBP among female athletes only. Kankaanpää et al. studied hip-extension and back-extension fatigability in subjects with chronic LBP and found that paraspinal fatigability was similar between groups, whereas the gluteus maximus fatigued more rapidly in the chronic LBP group. In addition, in a multifactorial cross-sectional study of 600 subjects with LBP, it was determined that hip-flexor, hip-adductor, and abdominal-muscle fatigability had a significant association with LBP. This research indicates the evolving body of evidence linking strength decrements of the hip region to LBP.
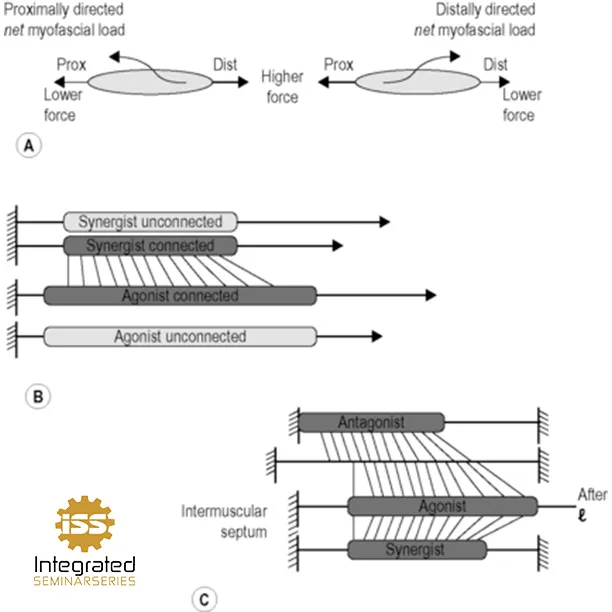
What if we consider “why” someone is weaker? What if we consider whether the patient is actually weaker or just presenting as weaker? If that seems like semantics, it’s not. Our current model of strength testing is an adaptation of the neurological model, wherein nerve function to a specific myotome is being tested. However, there is a lot more than neurology that contributes to strength in this scenario. For instance, joint position and the level of articular control.
Understanding Joint Position: Proximity to End Range and Centration for Optimal Strength Testing and Rehabilitation
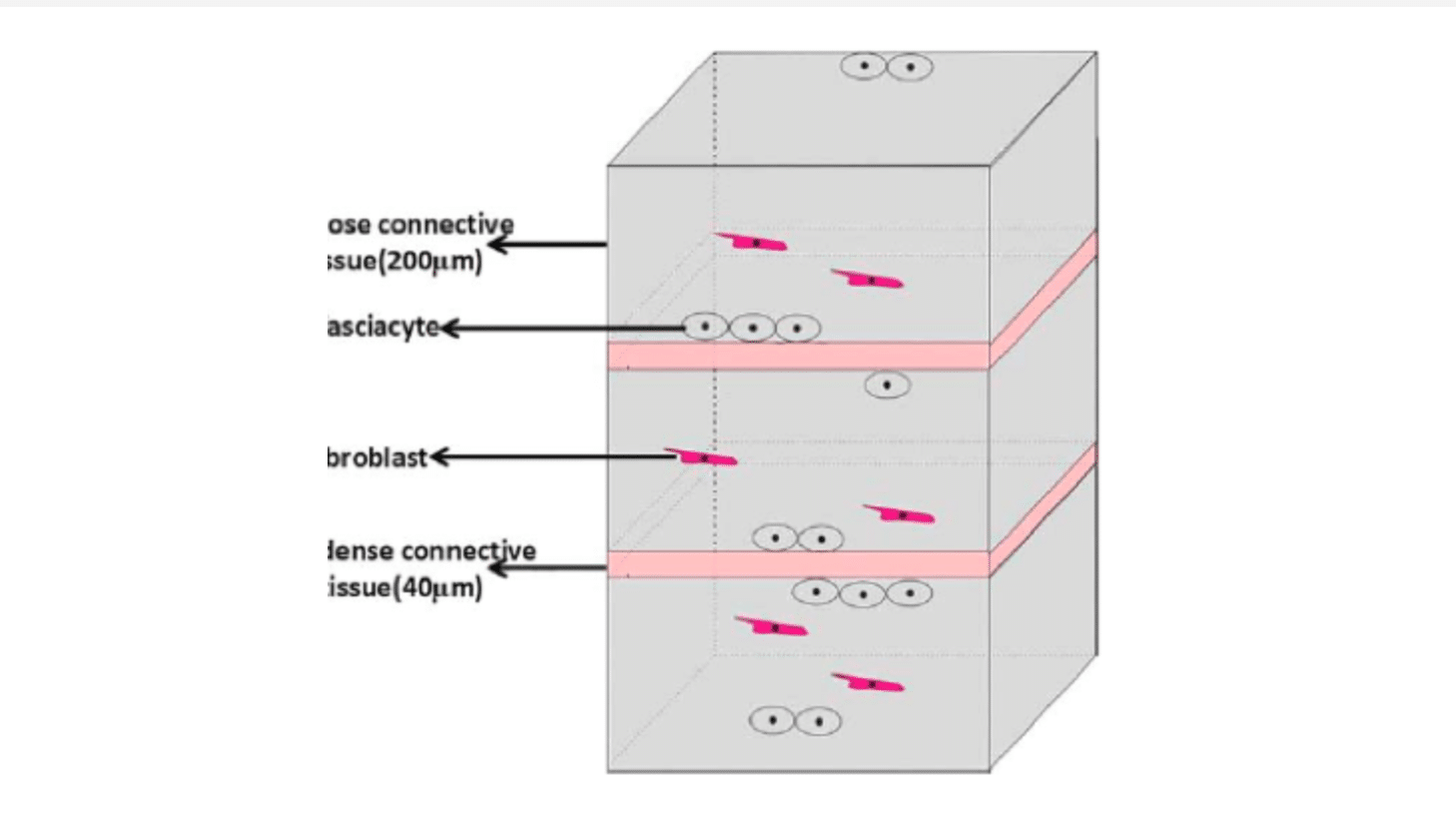
With respect to joint position, we have two variables to consider – proximity to end range and centration. Humans are weakest at end range, where they feel most vulnerable. Traditional strength testing of the gluteal muscles is done near end range of a joint with normal motion, but if you have a joint with limited range that testing will almost assuredly be at its end range when testing is performed. Concerning joint position, take the works of Burkart et al. regarding posterior or internal impingement of the shoulder. A capsule is meant to be the last bastion of stability when the neuromuscular system has failed, however when pathologically tight for whatever reason (typically driven by a lack of neurological control causing connective tissue tightness) it becomes a creator of aberrant motion my shifting the axis of rotation and pulling the joint out of centration.
“Joint centration or neutral joint position occurs when joint surface congruency and muscles that support the joint are at their optimal mechanical advantage throughout the range of motion and thus are able to produce varying forces according to the required skill.”
- Frank, Kobesova, and Holar, 2013
This mechanically disadvantageous position will cause a patient to test as weaker on a traditional muscle test. (Not to dive down too many rabbit holes at once but consider the repercussions of strengthening this poor pattern of movement and control. This is an incredibly important discussion to have, but also one I will table for a different day/post.) Decentration (the lack of centration) occurs near end ranges as the capsule is being tensioned, so testing a gluteal muscle at end range will certainly cause this phenomenon to occur.
Articular control, or lack thereof, will result in a similar joint decentration, and thus it will likewise produce false positives insofar as weakness is concerned. If a joint has proper control and can stabilize itself dynamically (see our previous blog post on the isometric end range training for additional insight and strategies to address this) we rely instead on passive restraint. As the large prime movers exert their influence across a joint, they exceed the capacity of the local stabilizing program and cause the joint to move. This movement is in turn mitigated by the capsule and ligaments. Centration only exists in a scenario where active control is achieved, which means they joint becomes decentrated and the therapist testing the patient finds weakness.
An excellent synopsis of this comes from the incomparable Shirley Sahrmann in her 2009 publication:
“Suboptimal function of the hip might result in an alteration of the mechanics of the lumbopelvic region. Such alterations contribute to low-magnitude loading of the lumbopelvic region and accumulation of tissue stress that, over time, contributes to tissue injury. For example, limited hip-rotation ROM resulting from shortened muscles, a stiff joint capsule, or a bony abnormality might contribute to compensatory movement in the lumbopelvic region. Such compensation could result in the lumbopelvic region’s moving more often during activities that require hip rotation, such as a golf swing or a racquet stroke. Altered coordination of hip and lumbopelvic- region movement could also result in an increase in lumbopelvic-region movement even when hip ROM is not limited. For example, during a test of active hip lateral rotation, the lumbopelvic region might move early in the hip motion secondary to altered hip- and trunk-muscle- recruitment patterns. In both examples, the increase in lumbopelvic-region movement could contribute to an increase in low-magnitude loading of tissue, microtrauma, LBP symptoms, and potentially macrotrauma.”
We will dive deeper into these concepts in later posts but suffice it to say there is clearly a link between anatomical segments, both in direct proximity and further up and down the chain from a biomechanical perspective.