We have referenced the term “Regional Interdependence” or “RI” multiple times, and alluded to its meaning, but what is RI? The term was originally coined by Wainner et al. in 2007, however Erhard and Bowling hinted at this concept in 1977.
“Dysfunction in any unit of the system will cause delivery of abnormal stresses to other segments of the system with the development of a subsequent dysfunction here as well” – Erhard and Bowling, 1977
The more recent presentation by Wainner came by way of a literature review wherein they noticed that regions of the body were linked from a musculoskeletal standpoint.
“With respect to. musculoskeletal problems, regional interdependence refers to the concept. that seemingly unrelated impairments in a remote anatomical region may. Contribute to, or be associated with, the patient’s primary complaint” –Wainner et al, 2007
Reconsidering the Biomedical Model for Musculoskeletal Disorders
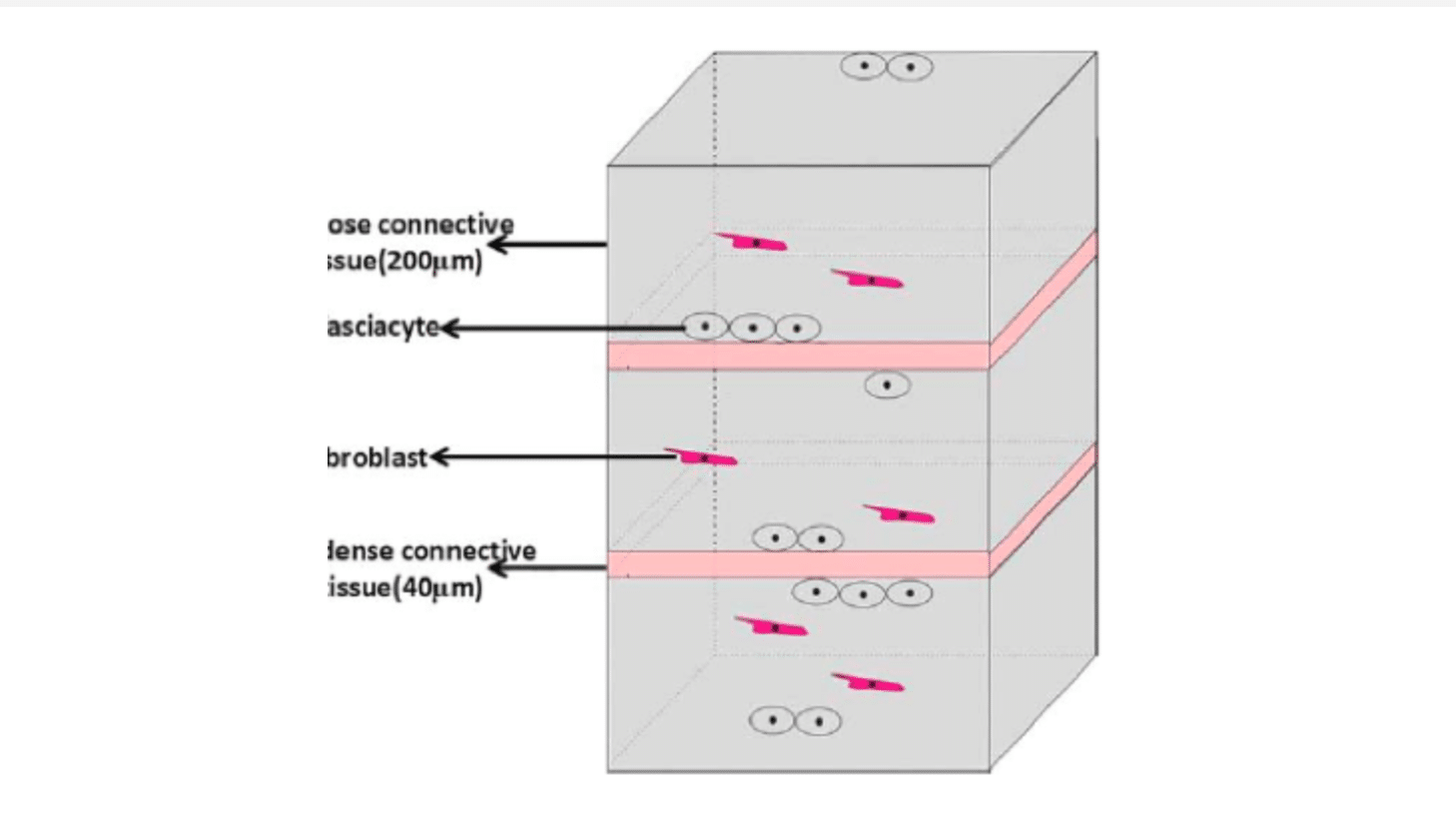
A wider net has also been cast by Bialosky et al. who suggest any system that affects a change in physiology should be considered, specifically somatovisceral and biopsychosocial inputs. This biomedical model of disease has served as the foundation for assessment and treatment and as a primary model for managing patients with musculoskeletal disorders. In this model, clinical management decisions are predicated on the identification of a pathoanatomical source tissue. The issue lies in the fact that interventions and treatment plans focused upon a single pathological structure can often result in poor outcomes, particularly with spinal disorders for which a pathoanatomic source tissue cannot be identified in the majority of cases as both Waddell and Bogduk commented on previously. Indeed, clinical decision making based on a single pathological finding has been credited by Waddell as contributing to these poor results. As such, the biomedical model should be expanded to include identification of other factors or regions that may contribute to the patient’s complaints. The RI model of assessment and treatment provides a framework to incorporate this expanded focus.
From Inman and Saunders in 1944 and Slocum in 1959, to more current iterations of RI from Cleland et al., Fernandez-de-las-Penas et al. and Gonzalez-Iglesias et al., there is a sizeable amount of literature on the subject of Regional Interdependence. Let us have a look at these published works before considering the mechanisms by which they affect their response in greater detail.
Lower body Regional Interdependence
Most of the literature assessing the lower extremity supporting the concept of RI is related to the lumbopelvic region. Low back pain has been positively associated with hip osteoarthritis, fractures, and following total hip replacement surgeries. Additionally, Stupar et al. have also demonstrated a positive relationship between low back pain and the presence of knee osteoarthritis. A positive association has also been found between decreased strength, neuromuscular control, range of motion, and mobility of the lower quarter with the presence of low back pain and impairments. A relationship between the foot and ankle and the lumbosacral region has been proposed in publications by Cibulka, along with Rothbart and Estabrook. Likweise, Kosashvili et al. demonstrated that a positive correlation exists between pes planus and low back pain. Similarly, Brantingham et al. established a positive relationship between ankle impairment and lumbar spine pain.
While the preponderance of literature has focused on the lumbopelvic region, there have also been several recent publications related to the knee. Powers, a prolific author in this realm whose impact on understanding knee pain cannot be overstated, has suggested that proximal factors such as hip impairment may play a contributory role in knee injuries. Bogla et al., Finnoff et al., Souza et al., and Rowe et al. have all demonstrated that deficits in hip strength and abnormal hip mechanics are positively correlated with knee pain. Although it is common clinical practice to assess and treat the foot and ankle in patients with other lower quarter impairments, very few studies aside from those mentioned previously have looked specifically at the influence that the ankle or foot can have on outcomes related to the hip, pelvis, or lumbar spine. Moreover, not assessing whether these sites, or potentially more than one site, is influencing the lumbar spine is almost as dangerous as not taking these factors into account. We need to assess all potential areas creating overload, to ensure that we treat only those areas that are contributing to the problem but also to elucidate that we have captured every variable responsible.
Upper body Regional Interdependence
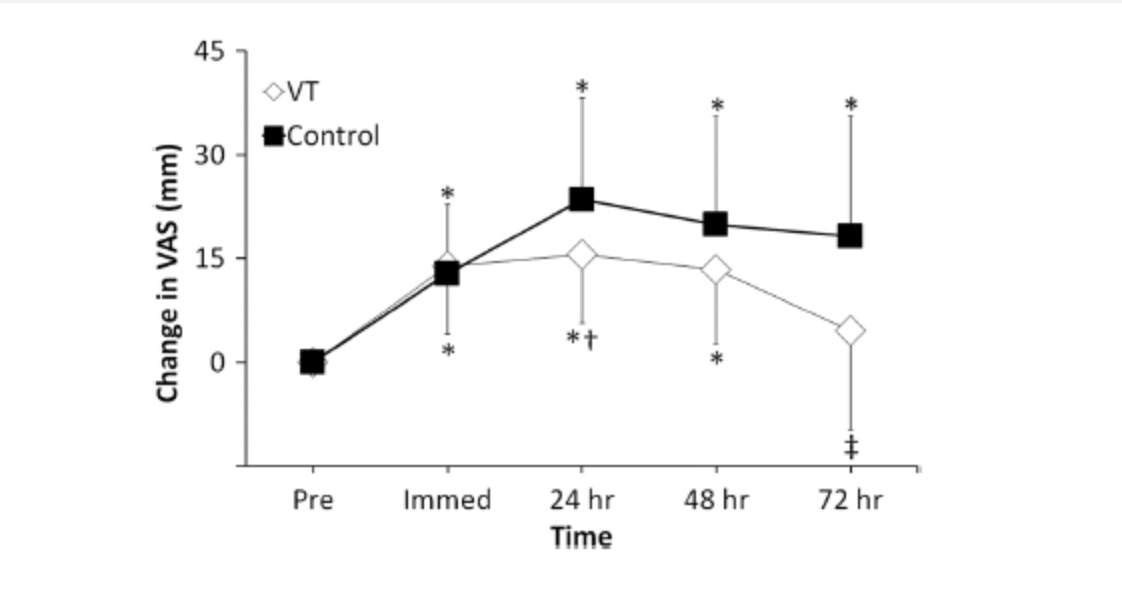
As with the lower body, the majority of studies assess the relationship of the spinal regions as well as the spine in relation to the upper extremity. Studies by Cleland et al. and Gonzales-Iglesias et al. linking cervical pain to thoracic interventions have been mentioned previously. Additionally, Strunce et al., Boyles et al., and Mintken have demonstrated that interventions focused on the thoracic spine have the potential to alter shoulder symptoms (see our blog The Link Between Thoracic Spine Mobility and Shoulder Pain for a more in-depth look at this element). Yoo et al. demonstrated that sympathetic blocks at the thoracic spine could improve upper extremity neuropathic pain while Berglund et al. found that pain and dysfunction of the thoracic spine is positively correlated with the presence of lateral elbow pain.
Less prevalent are those studies dealing with impairments in the cervical spine and upper quarter. Berglund et al. surveyed subjects with lateral elbow pain and found 70% of subjects also reported pain in the cervical and thoracic regions compared to 16% in the asymptomatic control group. Vicenzino et al. found that cervical manipulation caused a decrease in pressure pain threshold and increases in grip strength in subjects with lateral elbow pain. In a similar vein, Suter et al. demonstrated an increase in bicep muscle strength and a decrease in muscle inhibition following cervical manipulation.
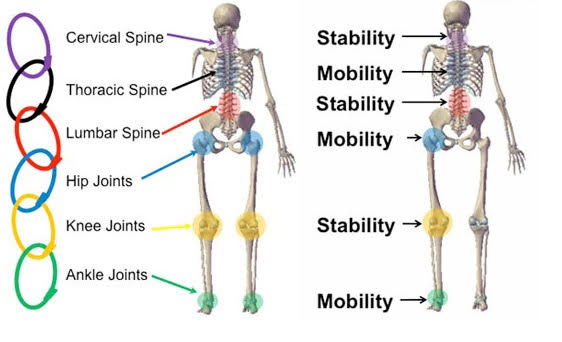
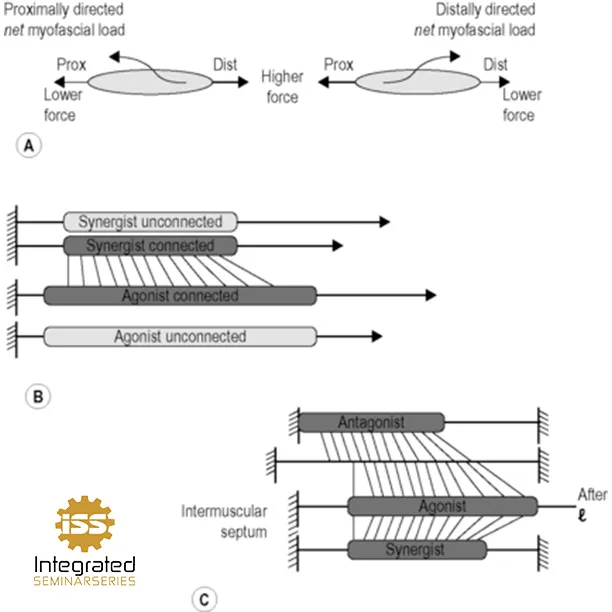
The Biomechanical Link: The Kinetic Chain Concept
From a mechanistic standpoint, how are these seemingly unrelated segments actually linked? If we look at the pioneering work of Steindler, you can see that he proposed a mechanism based on a kinetic mechanical engineering model. He termed this relationship the ‘Kinetic Chain’ and in his model, he describes the body as a series of interconnected joints where the movement of one joint directly effects the movement of other joints above and below, which in turn can effect those even further down this proposed chain. This model is thus based primarily upon the biomechanical relationship between regions of the body. For example, decreased dorsiflexion in the ankle mortise joint can produce biomechanical compensatory changes in knee, hip, and lumbar spine. More recent literature demonstrating interdependent relationships between the thoracic spine/cervical spine and the hip/knee are both examples of this potential biomechanical link. Joints that do not contribute to the magnitude that is required for efficient movement pass that demand along the chain, forcing these proximal or distal areas to perform additional work. Think of the patient with adhesive capsulitis that you ask to abduct their arm – the typical response involves movement at the glenohumeral joint that quickly reaches end range, translating to the scapulothoracic joint, thoracic spine, and into the lumbar spine. While this is potentially a more robust example than you would see outside of frozen shoulder, it nonetheless speaks to the mechanism of how aberrant mechanics in one joint are compensated for at other articulations.
Understanding Movement as a Shared Responsibility: Implications for Therapists and Strength Coaches
The key here is that we do not move in isolation, and as such, movement is a shared responsibility not only amongst various systems (myofascial, neurological, hematological, etc.) but also across various joints. Grasping a cup is not the sole responsibility of a hand – the elbow, wrist, shoulder, scapula, and thoracic spine, in addition to the fingers and thumbs, are required to perform this action. If you are standing while performing this task, then the lumbar spine, hips, and the whole lower extremity are involved even if only maintain vertical positioning a provide a base from which the arm can operate.
What does this mean for therapists and strength coaches? Two very important things. First, we cannot assess in isolation. Second, just as we cannot assess in isolation, we can treat/train/rehab in isolation. We do not move in isolation and as such any attempt to get overly myopic with assessment is likely missing out on important contributors. Likewise, if we attempt to ameliorate polyarticular processes with monoarticular solutions, we are missing a big part of the plan of management. The ultimate expression of what a human is capable of are the everyday, polyarticular movements that brought most people into the clinic in the first place. “I can’t run because my knees hurt”, or “every time I swing a golf club, I get a sharp pain in my posterior shoulder.” So while initial interventions concentrate on building monoarticular integrity, once established, management must focus on biarticular/biregional and then polyarticular/polyregional exercises to have context and ensure those everyday activities are performed optimally and without pain or limitation.